By Nora Marino, Health Policy Scholar at NACCHO and current Master in Public Health candidate at the University of Minnesota School of Public Health
NACCHO would like to thank Dr. Merritt Schreiber, Associate Professor at UC Irvine School of Medicine and UC Irvine Medical Center, Elsie Kusel of Alameda County Emergency Medical Services Agency, Sandra Shields of Los Angeles County DHS and Cathy Stout of MHMR Tarrant for their contributions to this blog.

Natural disasters, terrorist attacks, and other public health emergencies have wide-ranging implications on a community, so it is important for local health departments (LHDs) to continuously promote emergency preparedness planning. While most plans incorporate policies and procedures, such as the activation of the incident command system, many tend to overlook the mental and behavioral health needs of a community. One reason for this may be due to existing barriers such as the lack of time and resources needed to implement mental health triage into emergency plans. Existing models like the Psychological Simple Triage and Rapid Treatment (PsySTART), which is used to triage the general population, and the Anticipate Plan Deter (APD) Responder Resilience Program, which monitors emergency personnel responding to a disaster, are available for utilization for both state and local health departments, as well as hospitals systems.
PsySTART – Addressing the Mental Health of the Community
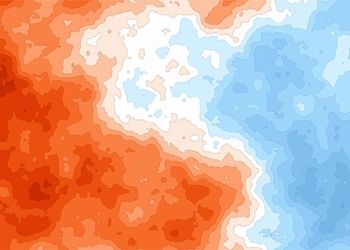
When disasters occur, individuals are not only at risk for physical injuries, but can also experience emotional and psychological injuries. Because of this, it is vital that communities not only monitor their population’s emotional stability, but also provide the appropriate services needed when responding to and recovering from an event. The PsySTART model, an evidence-based mental health response system, allows communities to build resiliency before, during, and after a disaster. This model uses information technology such as Geographic Information Systems (GIS) to provide real-time information on both specific locations and the severity of those who are experiencing a trauma. [1] The information collected is then used to triage those affected, allowing them to receive the appropriate services.
APD – Incorporating Emergency Personnel Mental Health
Emergency personnel and first responders put their own safety and emotional wellbeing aside to quickly respond during an emergency. As important members of the community, it is vital that these individuals engage in appropriate self-care before, during, and after a disaster. [2] This can be a challenge for some, since many first responders see themselves as immune to any emotional or psychological stress that may come with the job. The APD model, which ties into the PsySTART self-triage system, provides a framework for counties, cities, and hospital systems to develop mental health surveillance and support systems for emergency personnel. It also uses triage information as one aspect of a “personal resilience plan.” Overall, the APD model emphasizes the following:
- Anticipate: Understanding the stresses that emergency personnel experience in a disaster
- Plan: Developing an individualized, comprehensive, and strengths-based plan for emergency personnel and their family to use during an emergency
- Deter: Creating a system for emergency personnel to self-monitor themselves for emotional and psychological stability during and after a disaster. [2]
While disaster mental health is an emerging concept for many health departments, the following agencies used grant funding from the Hospital Preparedness Program to incorporate PsySTART, APD and other models into their emergency preparedness plan.
Los Angeles County
In 2009, the Emergency Medical Services Agency in Los Angeles County developed “train the trainer” classes on how to incorporate mental health into disaster planning. Nurses, social workers, and hospital staff from approximately 80 hospitals and 33 clinics participated, giving them the opportunity to train other staff members within their hospitals and clinics. In addition, Los Angeles County also provides a 30-minute APD training to health care workers to assist emergency personnel in developing an individualized disaster preparedness plan that will increase their resiliency while responding to a disaster. In the future, they hope to continue to find innovative ways to increase the number of hospitals and clinics that are using these mental health preparedness models.
Tarrant County
In Tarrant County, MHMR Tarrant works with North Central Texas Trauma Regional Advisory Council (NCTTRAC) to develop APD: Responder Resilience, which provides a smart phone app for emergency personnel to confidentially report their exposure to traumatic events. Following a traumatic event, it is important to objectively and confidentially measure exposure instead of symptoms because symptoms may take weeks or years to surface and responders are less likely to report them. After responders report exposure, the app helps them to identify personal impact and connects them to available resources. The information reported in the app then becomes aggregate data that is used to inform real time behavioral health responses and interventions. Examples of interventions include alternating shift assignments during a prolonged disaster response and reminding emergency personnel of their personal mental health preparedness plan developed in the APD training.
Alameda County
In California’s Alameda County, the Emergency Medical Services Agency provides a comprehensive orientation for paramedics who are new to either the field or the county. The training emphasizes topics that are unique and important to the region such as, treatment of cardiac arrest, how to work with underserved and diverse populations, and how paramedics can care for their own mental health when exposed to a trauma. In the future the county hopes to increase their relationships with mental health providers, as well as increase providers’ understanding of the unique needs of emergency personnel and how to best provide services to this population.
How is your LHD incorporating mental and behavioral health into emergency plans? Leave us your comments in the section below.
References:
(1) Schreiber, M. (2010). The PsySTART Rapid Mental Health Triage and Incident Management System. Retrieved from http://www.cdms.uci.edu/disaster_mental_health.asp
(2) Schreiber, M. (2014). APD Trainer Guide for LAC EMS Agency.